Imagine a digital system that doesn’t wait for instructions but instead, understands your business goals, learns from real-time feedback, and takes independent actions to get the job done.
Read More

If your healthcare business still relies on spreadsheets for billing, it’s probably time for a reality check. The world has moved on, and the ones still wrestling with manual claim submissions are watching their reimbursements crawl while others race ahead with automation. That’s the not-so-gentle nudge to start thinking about how to build an AI medical billing software that can actually keep up with the pace of modern healthcare.
Between rising patient volumes, changing regulations, and unpredictable payer rules, billing teams have their hands full. Errors creep in, claims get rejected, and before you know it, cash flow is gasping for air.
The antidote? AI medical billing software development that learns, predicts, and automates your entire billing ecosystem.
Building such a system is about survival in an industry where a few delayed claims can send revenue cycles spiraling. Whether you’re running a hospital, clinic, or healthcare startup, learning to develop AI billing system for healthcare operations is your ticket to staying ahead.
And here’s where things get interesting. When you make AI medical billing applications for insurance and healthcare startups, you’re building an intelligent assistant that reduces human error, processes claims faster, and keeps compliance nightmares at bay.
Ready to see how the smartest players in healthcare are automating their way to better profits and peace of mind? Let’s dive into how you can join them.
If the words "medical billing" make you think of endless spreadsheets, compliance paperwork, and a few mild headaches, you’re not alone. That’s exactly why healthcare innovators are rushing to build an AI medical billing software that can turn chaos into clarity.
So, what exactly are we talking about? Let’s break it down.
An AI medical billing software is a smart digital system designed to manage, automate, and optimize every part of the healthcare billing process. Powered by generative AI and machine learning, it’s like hiring a 24/7 billing specialist who never forgets a code, never gets tired, and learns from every claim processed.
Instead of relying on manual entry and human oversight, AI medical billing software development focuses on integrating technologies like machine learning (ML), natural language processing (NLP), and robotic process automation (RPA) to handle repetitive, rule-based billing tasks.
In plain words, it reads, interprets, and acts. From pulling data out of patient records to generating accurate claims, it does the heavy lifting while your team focuses on care, not codebooks.
Here’s where the magic happens. Artificial intelligence automates and evolves, the core of every AI medical software development initiative lies in making processes faster, more accurate, and self-learning.
Essentially, AI makes billing faster and smarter.
Now, let’s look under the hood of how an intelligent billing engine works in real-world scenarios.
| Stage | What Happens | AI’s Role |
|---|---|---|
|
Data Intake |
The system collects data from EHRs, patient management systems, and payer databases. |
NLP cleans and structures unformatted text from reports or prescriptions. |
|
Code Selection |
Medical codes (ICD, CPT, HCPCS) are applied based on diagnosis and procedures. |
AI matches clinical context to codes with precision, reducing manual input errors. |
|
Claim Generation |
Claim forms are built and verified before submission. |
ML models verify claim data, cross-check payer requirements, and flag missing info. |
|
Claim Submission |
Claims are routed to insurers or clearinghouses. |
Automated claim routing based on payer rules and policy logic. |
|
Payment Posting |
Once payment or denial is received, it’s recorded automatically. |
AI reconciles payments, tracks denials, and updates the ledger. |
|
Analytics & Optimization |
Trends and financial performance are analyzed. |
Predictive analytics identify patterns in denials, payment delays, or revenue dips. |
Each stage builds on the previous one, creating a feedback loop where the software keeps learning and improving.
Here are the main pillars that keep your AI medical billing software development project running smoothly.
These components are the backbone of your system. The tech stack we’ll discuss later will give them their superpowers, but these are the gears that keep the machine turning.
Building an AI billing solution is like training a digital workforce. It learns your language, follows your rules, and helps your team breathe easier. But before you get into AI medical web development, let’s understand why businesses should invest in AI medical billing software development and what the market has to say about this goldmine of opportunity.
You've seen the components, now let experts of healthcare automation fine-tune them.
Build with Biz4GroupIf your healthcare organization or medical-billing outfit is still holding out on innovation, you’re paying a hidden tax. A tax of slower reimbursements, higher denials, and missed opportunities. Now is the time to develop AI billing system for healthcare, and here’s exactly how the market and pain-points make that clear.
These stats show a real opportunity. When you create AI-powered medical billing application, you’re stepping into a growing market with major inefficiencies to fix.
Here’s a table marrying the problems healthcare providers and payers face, with how a custom AI medical billing software helps turn things around:
| Pain Point | Business Benefit of Custom AI Medical Billing Solutions |
|---|---|
|
High denial rate (10 %+ of claims) |
Reduced denials, faster reimbursements, improved cash flow |
|
Manual code selection and human errors |
Accurate coding via AI/NLP, fewer disputes and reworks |
|
Slow claim processing and reimbursement delays |
Automated workflows, quicker claim submission and posting |
|
Aging systems and fragmented integrations |
Seamless integration with EHR/clearinghouse, improved operational efficiency |
|
Resource-intensive billing teams and staffing pressures |
Lower overhead, better utilization of talent, higher throughput |
|
Compliance risk with evolving regulations |
Built-in audit trails, regulatory updates, and AI-driven safeguards |
|
Poor visibility into revenue cycle data |
Real-time analytics dashboards, predictive insights for revenue forecasting |
These benefits tie directly into why healthcare organizations and startups need to make intelligent medical billing software. They’re not just software upgrades, they’re revenue engines.
Think of your billing system as a car. You can have the fanciest AI engine under the hood, but if it’s missing essentials like brakes or headlights, the ride is going to be rough. Before we get fancy with predictive AI, let’s talk about the features that make your AI medical billing software development project functional, compliant, and worth every penny.
These must-have features are the foundation of every successful automated healthcare billing software. They handle everything from data capture to claim submission, forming the backbone of smooth revenue cycle management.
| Feature | What It Is | What It Does |
|---|---|---|
|
Patient Information & Eligibility Verification |
A feature that validates patient demographics, insurance coverage, and policy status at registration. |
Prevents claim rejections by confirming insurance details before services are billed, ensuring only valid claims move forward. |
|
Medical Coding Assistance |
Integrated coding module aligned with ICD-10, CPT, and HCPCS standards. |
Suggests or auto-applies correct procedure and diagnosis codes, reducing manual errors and improving billing accuracy. |
|
Claim Generation & Scrubbing |
Automated system for building and verifying claims before submission. |
Detects incomplete or inaccurate claim data, cross-checks payer rules, and flags issues early to minimize denials. |
|
Automated Claim Submission |
Electronic claim filing system linked to payers or clearinghouses. |
Speeds up submission, reduces paperwork, and ensures every claim follows payer-specific requirements. |
|
Payment Posting & Reconciliation |
Module to automatically record payments, denials, and adjustments from payers. |
Keeps accounts up to date, accelerates cash posting, and ensures transparency in financial reporting. |
|
Denial Management & Appeals Tracking |
Tool for identifying, categorizing, and managing denied claims. |
Allows staff to analyze denial reasons, generate appeals, and track resolution progress efficiently. |
|
Reporting & Analytics Dashboard |
Real-time dashboard that visualizes claim statuses, payments, and revenue KPIs. |
Helps management monitor trends, predict bottlenecks, and make data-driven decisions for better cash flow. |
|
User Management & Role-Based Access |
Secure access control system defining roles for billing staff, administrators, and auditors. |
Ensures compliance with HIPAA and internal security policies by controlling who sees and edits sensitive data. |
|
Integration with EHR and Practice Management Systems |
Connects billing functions with existing clinical and administrative software. |
Eliminates redundant data entry, ensures seamless information flow, and improves efficiency across departments. |
|
Audit Trail & Compliance Logging |
Built-in system that records all user actions, edits, and claim activities. |
Supports internal audits and regulatory reviews by maintaining full transparency and accountability. |
These features form your billing software’s DNA. Without them, even the smartest AI model would struggle to make an impact. But once these basics are in place, that’s when things get exciting.
Because up next, we’ll go beyond the fundamentals into the world of predictive analytics, NLP-driven coding, and self-learning systems that redefine how you make intelligent medical billing software.
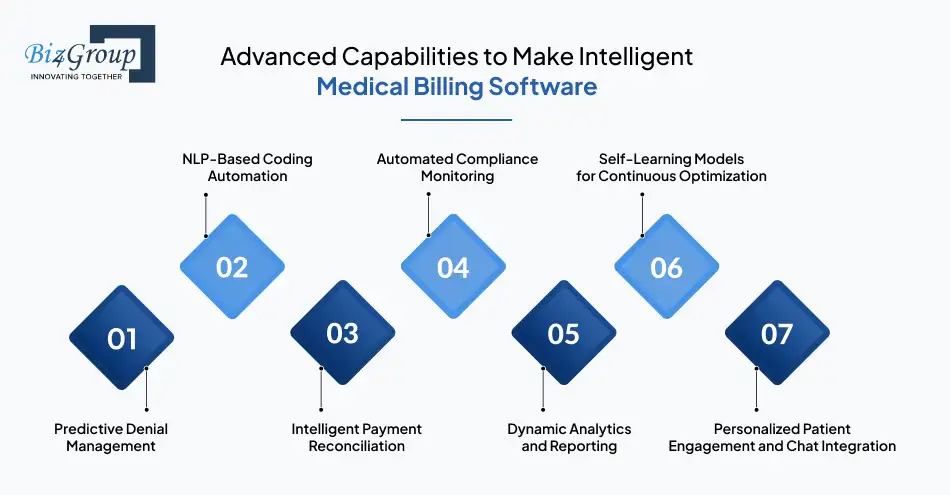
Once the foundation is set, it’s time to add the features that make your AI medical billing software development truly powerful. These capabilities transform billing from a reactive process into a proactive, data-driven system that gets smarter with every claim processed.
Below are the advanced functions that bring intelligence, efficiency, and sophistication to your AI-powered medical billing application.
Imagine if your billing software could warn you before a claim got rejected. That’s predictive denial management at work. AI models analyze patterns from historical claims and payer responses to forecast which submissions are at risk of denial. This helps billing teams fix issues before sending them out. This feature also strengthens your bottom line by cutting lost revenue and improving claim accuracy.
Each denied claim costs an average of $25 to $118 to rework. Predicting denials early means more approvals, fewer write-offs, and faster reimbursements.
Coding is complex, time-consuming, and prone to human error. Natural Language Processing (NLP) changes that. The system reads physician notes, extracts relevant medical terms, and automatically assigns the correct ICD, CPT, or HCPCS codes. The result? Coding accuracy skyrockets, and human oversight drops dramatically.
This not only helps avoid under-coding or over-coding but also ensures faster claim turnaround. The system keeps learning from coding decisions, getting sharper with every new entry.
Traditional payment posting often feels like a game of guesswork. AI turns that into science. By matching payer remittances with claims automatically, it identifies discrepancies, flags underpayments, and even suggests corrections. This process ensures revenue leakage is caught before it becomes a financial drain.
No, it’s not about replacing your accounting team. It’s about giving them a smart assistant that never misses a number.
Healthcare billing lives under the constant shadow of compliance. AI ensures your system is always up to date with the latest coding and regulatory changes. Whether it’s HIPAA, ICD updates, or payer-specific policies, the software keeps track automatically. This reduces the risk of violations and provides peace of mind to both administrators and auditors.
Gone are the days of static Excel sheets. Intelligent billing software thrives on visual dashboards and real-time analytics. AI identifies bottlenecks, tracks performance KPIs like denial rates or reimbursement cycles, and provides actionable insights. It reports what’s happening and tells you why it’s happening and what to do next.
Every claim processed is another lesson for your AI. Self-learning models continuously analyze past transactions and feedback loops to improve prediction accuracy and decision-making. Over time, this results in a system that adapts to payer behavior, healthcare trends, and even internal workflow changes.
Here’s where things get exciting and personal. Apart from backend processing, modern billing is also about patient communication and engagement.
This is where Biz4Group’s Select Balance stands out.
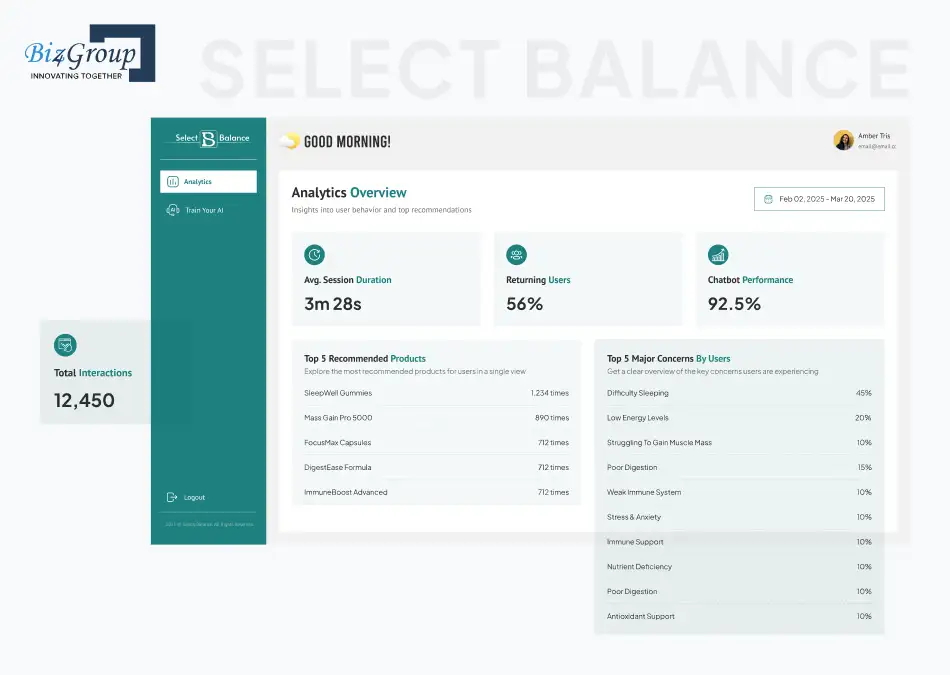
As a leading AI chatbot development company, we developed Select Balance, an AI-powered chatbot that engages users through a friendly quiz or natural conversation, helping them find the right health supplements tailored to their needs. The system integrates seamlessly with a live database to provide instant, accurate recommendations, all in real time.
Now, imagine this level of personalization applied to billing. An AI chatbot can guide patients through payment plans, claim statuses, or eligibility queries without human intervention. It builds trust, reduces support load, and enhances user satisfaction. This is the kind of innovation we’ve explored deeply through our AI medical chatbot development projects, where conversational AI becomes a bridge between automation and empathy.
Why it shines:
These advanced features are what separate an ordinary billing tool from an intelligent, adaptable system that feels almost alive. They make your operations faster and future-proof.
Next, we’ll unpack how to actually build one. The process, the flow, the steps, and yes, the secrets that make a world-class AI medical billing software development project successful from day one.
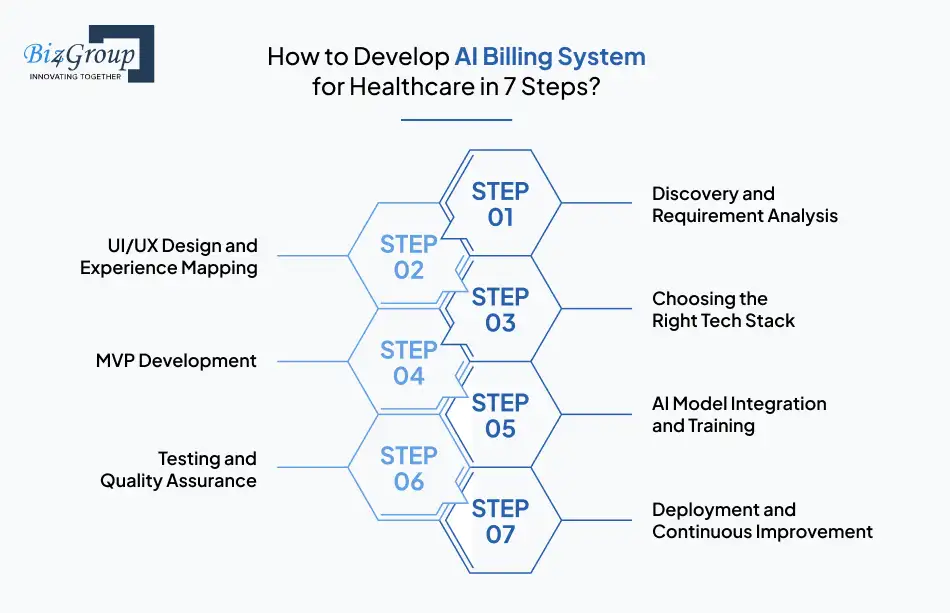
You can’t just throw a bunch of developers, data, and algorithms together and expect a fully functional billing marvel to pop out. Building a healthcare-grade, intelligent billing system requires strategy, precision, and the right sequence of steps.
Let’s walk through how you can create an AI-powered medical billing application that’s reliable, scalable, and loved by both accountants and doctors alike.
Before writing a single line of code, you need clarity. This phase is about understanding who you’re building for, what challenges they face, and how your software will fix them.
Remember, the better your discovery, the smoother every step that follows.
No matter how smart your system is, if users find it confusing, they’ll abandon it faster than a bad webinar. A reliable UI/UX design company helps keep everything intuitive, clean, and efficient.
Good design improves adoption rates and reduces training costs.
Also read: Top 15 UI/UX design companies in USA
Tech stack development determines your software’s speed, security, and scalability.
Suggested Stack Overview:
| Layer | Technology | Purpose |
|---|---|---|
|
Front-End |
React.js, Angular, Vue.js |
Associate with a top-notch React.js development company for interactive and responsive interfaces |
|
Back-End |
Node.js, Python (Django/Flask), Java Spring Boot |
Manages business logic, APIs, and integrations |
|
Database |
PostgreSQL, MongoDB |
Stores patient, claim, and transaction data |
|
AI/ML Frameworks |
TensorFlow, PyTorch, Scikit-learn |
Drives predictive modeling and NLP coding automation |
|
NLP Tools |
SpaCy, NLTK |
Enables natural language understanding for coding and notes |
|
Cloud & DevOps |
AWS, Google Cloud, Docker, Kubernetes |
Enables scalability and CI/CD pipelines |
|
Security & Compliance |
OAuth 2.0, SSL, encryption libraries |
Ensures data privacy and HIPAA compliance |
|
Integration APIs |
HL7, FHIR, REST APIs |
Facilitates secure communication with EHRs and payers |
Your stack should match your goals. Partner with a leading Python development company for AI-heavy modules, an experienced Node.js development company for scalable APIs, and AWS for smooth cloud deployments.
Building an MVP (Minimum Viable Product) is how you validate your vision in the real world without overspending.
An MVP helps you avoid the classic “feature overload” trap. Start lean, validate fast, and improve continuously.
Also read: Top 12+ MVP development companies in USA
This is where your software starts flexing its intelligence.
Remember, AI is a living system that grows smarter with time and data.
Testing AI billing software is like tuning a race car, every component must run perfectly in sync.
Your users should trust your system enough to let it handle millions in revenue without blinking.
Deploy your custom AI medical billing solutions on your preferred cloud platform and monitor performance in real-time.
This is also where your post-launch partner matters. Speaking of...
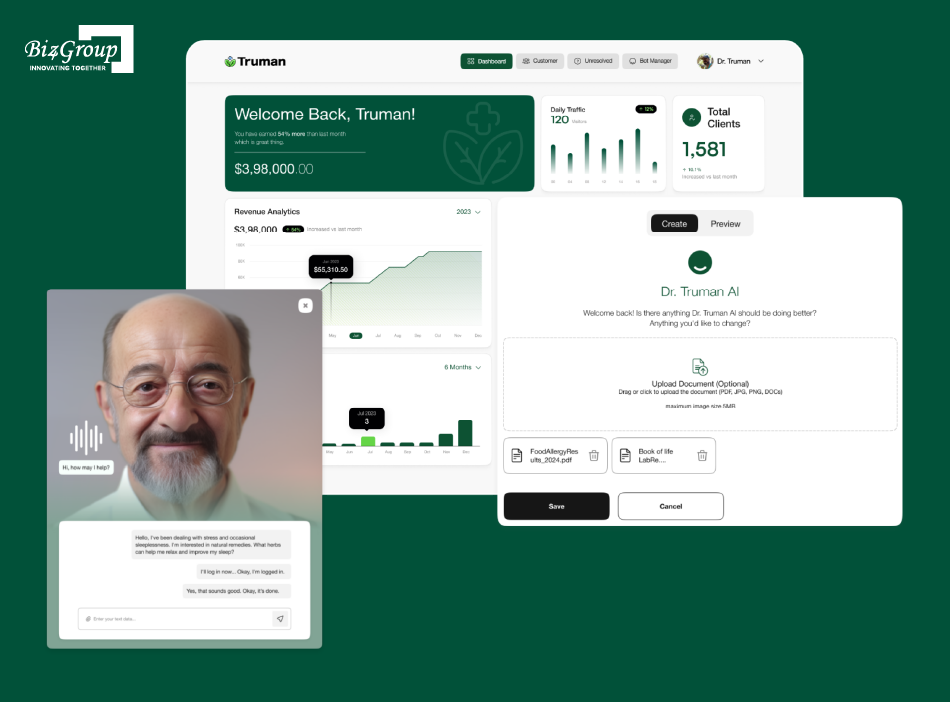
When we talk about turning ambitious ideas into high-performing AI healthcare products, our Dr. Truman AI Avatar project is the gold standard.
Dr. Truman wanted a living, breathing AI companion that could deliver personalized health advice, product recommendations, and seamless eCommerce integration. Our team delivered an AI-enabled wellness companion that feels as real as having a virtual doctor in your pocket.
Here’s what made it shine:
This project exemplifies what happens when creative design meets intelligent engineering. The same strategic approach, building AI that learns, adapts, and integrates seamlessly, is exactly what sets a successful medical billing platform apart.
When you develop AI billing system for healthcare, the goal is transformation. Build it once, keep refining it, and let it evolve with your users, just like we did with Dr. Truman’s digital avatar.
You've just read how the pros do it. Now it's your turn to build something extraordinary.
Get in Touch with UsHealthcare billing is extensively about trust. Patients trust providers with their data, providers trust systems with their revenue, and regulators trust you to play by the rules. That’s why security and compliance sit at the core of AI medical billing software development.
Below are the key principles, practices, and frameworks that keep your automated healthcare billing software bulletproof from data breaches, non-compliance fines, and operational disruptions.
Also read: How to develop HIPAA-compliant AI medical transcription software
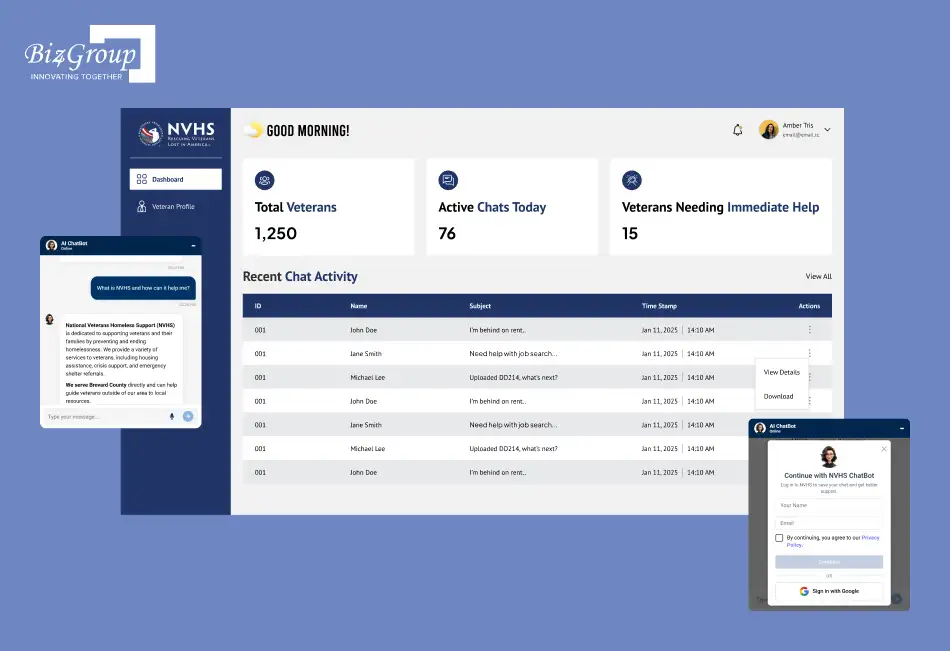
Biz4Group has firsthand experience building AI systems where compliance isn’t just technical, but also human. Our NVHS chatbot for homeless and at-risk veterans is a perfect example.
We built NVHS as an AI agent development company and learnt that secure AI systems aren’t about locking data away. They’re about enabling help responsibly. The same principle powers every automated healthcare billing software we build at Agentic AI Development Company
Next, we’ll pull back the curtain on a question every healthcare organization asks early in their AI journey, what does it actually cost to build one?
Let’s talk numbers. Building a full-scale AI medical billing software development solution is a serious investment, but one that pays off in efficiency, revenue, and long-term scalability.
On average, the cost to build an AI medical billing software ranges between $45,000-$200,000+, depending on complexity, AI integration services, and scalability goals. Here’s a quick snapshot of what that investment looks like across different stages of growth.
| Stage | Scope | Estimated Cost |
|---|---|---|
|
MVP (Minimum Viable Product) |
Core billing automation, claim submission, and basic AI coding features |
$45,000-$70,000 |
|
Advanced Level |
Predictive analytics, denial management, AI-powered reporting, multi-payer integration |
$80,000-$130,000 |
|
Enterprise Level |
End-to-end AI automation, NLP coding, compliance modules, scalability for multiple locations |
$150,000-$200,000+ |
Each level represents more intelligence, automation, and long-term ROI. Now, let’s break down where your money actually goes, what hidden costs can surprise you, and how to keep your investment optimized for maximum returns.
When you develop custom AI medical billing solutions for hospitals and clinics, several factors influence your total cost. Understanding them early helps you plan realistically and avoid unpleasant surprises.
The wider your feature set, the higher the cost.
Training AI on claim data, payer behavior, and billing patterns can take 4-8 weeks.
Integration with existing EHRs, clearinghouses, and insurance APIs is one of the most time-consuming components.
A good interface is an investment, not an expense.
A solid compliance module can save hundreds of hours in audits and legal reviews.
Not every expense shows up in your initial quote. Below are the costs that often sneak up later if not factored early.
| Hidden Cost | What It Involves | Potential Impact |
|---|---|---|
|
Third-Party API Fees |
Charges for external APIs like EHR, clearinghouses, or payment gateways |
Can add $500-$2,000/month |
|
AI Model Retraining |
Ongoing data updates and re-optimization of algorithms |
Adds 10-15% to annual maintenance |
|
Compliance Audits |
Periodic HIPAA or SOC2 audits |
$3,000-$8,000 annually |
|
Software Licensing |
Paid libraries or NLP frameworks |
$2,000-$6,000 per year |
|
Post-Launch Support & Updates |
Ongoing improvements and bug fixes |
$1,500-$5,000/month |
|
Data Migration |
Shifting legacy data to new system |
One-time $5,000-$15,000 effort |
These costs are part of the fine print that smart planning turns into predictable expenses.
Building an intelligent system doesn’t mean burning through your budget. Strategic decisions can keep costs lean while ensuring high performance.
Begin with a functional MVP to validate workflows and gather real user feedback. Gradually add advanced features like AI chatbots or predictive analytics.
This phased approach can reduce initial investment by 25-40% while maintaining forward scalability.
Cloud platforms like AWS HealthLake or Google Cloud Healthcare are far cheaper than traditional servers. You’ll save 30-50% on infrastructure management and upgrades annually.
Use AI-assisted QA tools to speed up testing cycles and reduce manual QA hours by 35-45%. Continuous integration (CI/CD) pipelines cut release times and minimize post-launch bugs.
Set aside 10-15% of your annual budget for maintenance, retraining AI models, and feature updates. Systems that evolve continuously perform 40% better in claim accuracy and compliance over time.
Building an AI-powered billing system isn’t cheap, but it’s worth every dollar when you measure the savings, speed, and accuracy it delivers. With clear planning and smart optimization, you can keep costs predictable and returns impressive.
Next, we’ll uncover how to measure the performance and monetize your AI medical billing software, because what’s the point of innovation if it doesn’t improve both your ROI and revenue stream?
You’ve built it. You’ve launched it. But how do you know your AI medical billing software development project is actually paying off? And more importantly, how do you turn that intelligent system into a sustainable revenue generator?
This section dives into the key performance indicators (KPIs) that prove your system’s worth and the monetization models that ensure your investment makes money.
KPIs are your reality check. These numbers tell you how efficiently your AI-powered medical billing application performs and where optimization is needed.
Core KPIs to Monitor:
| KPI | What It Measures | Why It Matters |
|---|---|---|
|
Claim First-Pass Rate |
% of claims accepted on first submission |
Higher rate = fewer denials, faster revenue cycle |
|
Claim Denial Rate |
% of claims denied by payers |
Tracks billing accuracy and AI model effectiveness |
|
Average Claim Processing Time |
Time taken from submission to reimbursement |
AI aims to cut this by 40-60% over manual processes |
|
Cost per Claim |
Average cost of managing one claim |
Should decrease as automation increases |
|
Revenue Cycle Efficiency |
Ratio of total collections to billed amount |
The ultimate indicator of billing performance |
|
AI Accuracy Rate |
% of correct AI predictions/coding matches |
Reflects the learning quality of your models |
|
User Satisfaction Score (CSAT) |
Feedback from billing teams and administrators |
A happier staff means better adoption and ROI |
Pro Tip: Benchmark these KPIs quarterly. Over time, you’ll see your AI’s impact compound, reduced claim turnaround, improved accuracy, and increased cash flow.
Your custom AI medical billing solutions should become a revenue stream themselves. Here’s how you can monetize effectively based on your business model and target audience.
Charge clients (clinics, billing companies, startups) a recurring monthly or yearly subscription fee.
Example: A SaaS billing platform serving 100 clients at $1,000/month nets $1.2M annually.
Charge per claim processed or per API call.
Average: $0.05-$0.15 per claim for high-volume users.
License your AI billing platform to other healthcare tech providers under their brand.
Licensing fees typically range from $25,000-$75,000 per year per partner.
Offer premium analytics dashboards powered by AI.
Provide integration modules (EHR, payer, or CRM) as optional paid add-ons.
Knowing your KPIs is one thing, translating them into profit metrics is another.
Use this simple ROI framework:
ROI (%) = [(Financial Gains - Total Investment) / Total Investment] x 100
Once you can measure it, you can monetize it, and once you can monetize it, your AI medical billing software development stops being a back-office function and becomes a front-line business driver.
Next, let’s discuss the challenges, risks, and mistakes businesses often make while trying to build intelligent medical billing software to automate claims, and how to dodge them like a pro.
Also read: Top 15 AI healthcare software development companies in USA
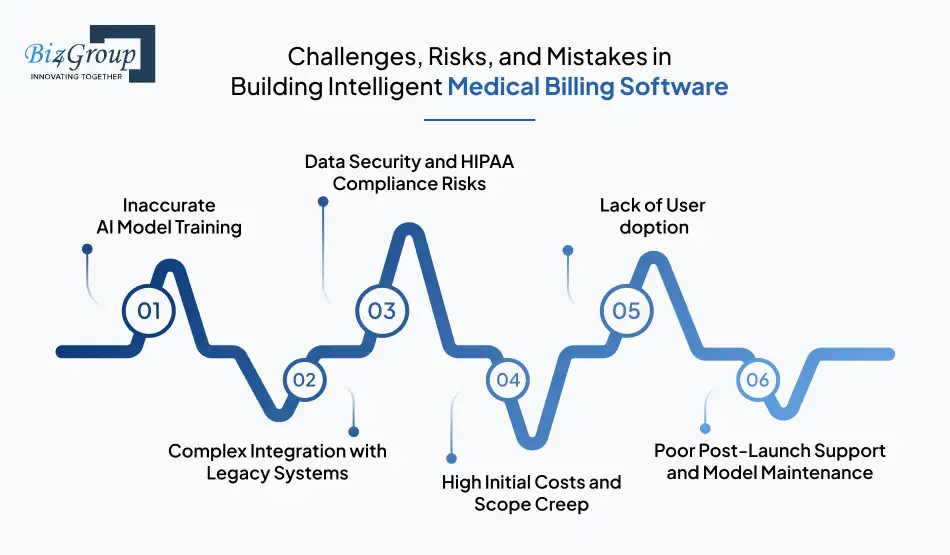
Building a smart, compliant, and scalable AI medical billing software is about precision. One missed compliance clause, one untrained AI model, or one poor integration can send months of work spiraling.
Let’s explore the common roadblocks teams face when they develop custom AI medical billing solutions for hospitals and clinics and how to overcome them before they become costly mistakes.
When your AI models are trained on inconsistent or insufficient data, they deliver flawed billing predictions, poor code mapping, and false claim rejections.
Solutions:
Most hospitals and billing companies rely on legacy EHR or practice management systems. Connecting modern AI software to outdated infrastructures can feel like teaching a flip phone to stream Netflix.
Solutions:
AI billing software handles vast amounts of sensitive patient data. One breach, and the financial (and reputational) damage could be enormous.
Solutions:
AI projects can snowball fast if requirements aren’t crystal clear from day one. Too many “nice-to-have” features early on can inflate costs and delay delivery.
Solutions:
Even the smartest AI system fails if users don’t trust or understand it. Billing teams often hesitate to rely on automation for compliance-heavy tasks.
Solutions:
AI systems evolve. Many companies launch, celebrate, and then forget the continuous learning part, leaving systems outdated and underperforming within months.
Solutions:
Facing these challenges early can mean the difference between a software that functions and one that dominates. When you plan your AI medical billing software development with these pitfalls in mind, you build a lasting competitive advantage.
Next, let’s shift focus to what’s ahead.
Partner with a team that's already fixed them for industry leaders and would do the same (and more) for you.
Talk to Our Experts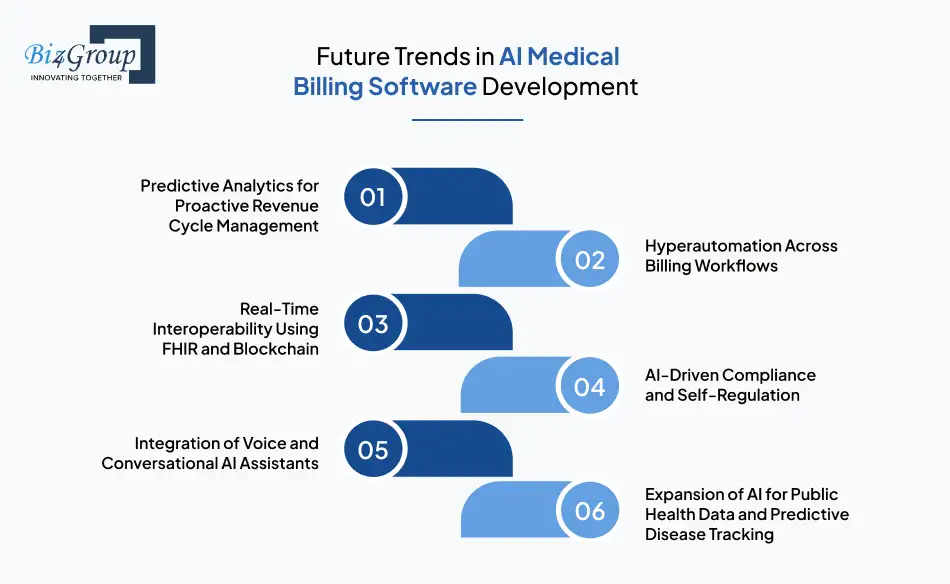
The world of healthcare billing is changing faster than ever, and AI is at the heart of it. What started as a solution to reduce manual work has evolved into a full-fledged intelligence ecosystem where algorithms learn, predict, and even communicate.
Let’s look at what’s shaping the future of AI medical billing software development, and how it’s redefining the healthcare revenue cycle for years to come.
Predictive analytics will soon help healthcare providers identify claim denials before they occur, forecast revenue dips, and recommend preventive actions. AI models will analyze historical data across payers and patient types to flag potential issues like missing codes or compliance mismatches. This proactive approach will improve first-pass claim rates by up to 60%.
Future billing systems will use AI, machine learning, robotic process automation (RPA), and intelligent document processing (IDP) together to automate every repetitive workflow. As hyperautomation takes over billing, expect similar intelligence to power broader ecosystems. In fact, AI hospital management software development is evolving alongside billing automation to unify administrative and financial workflows for complete operational efficiency.
With FHIR (Fast Healthcare Interoperability Resources) standards and blockchain integration, medical billing will become faster, more secure, and far more transparent. FHIR ensures that patient and claim data move smoothly between EHRs, payers, and clearinghouses. Blockchain adds an immutable layer of verification, reducing fraud, duplicate claims, and mismatched data entries. Together, these technologies promise a future where trust, speed, and accuracy become the default.
Expect future systems to self-audit their actions, automatically flagging non-compliant activities, documenting audit trails, and updating to match new billing laws in real time. Imagine a system that not only follows HIPAA or HITECH but predicts upcoming changes and adapts accordingly. That’s where AI in compliance is headed, reducing human effort while staying one step ahead of legal requirements.
The next frontier for intelligent medical billing software will be conversational. Voice-based billing assistants powered by NLP (Natural Language Processing) will make operations faster, hands-free, and far more intuitive. They’ll interpret voice commands, pull up analytics, and even generate reports on the fly. This evolution marks the end of traditional interfaces and the beginning of voice-first billing intelligence.
AI in billing will also contribute to broader healthcare intelligence. Data from billing systems will integrate with public health networks to track disease patterns, patient demographics, and treatment trends in real time.
This is where Biz4Group’s RdeXX becomes a shining example of innovation meeting purpose.
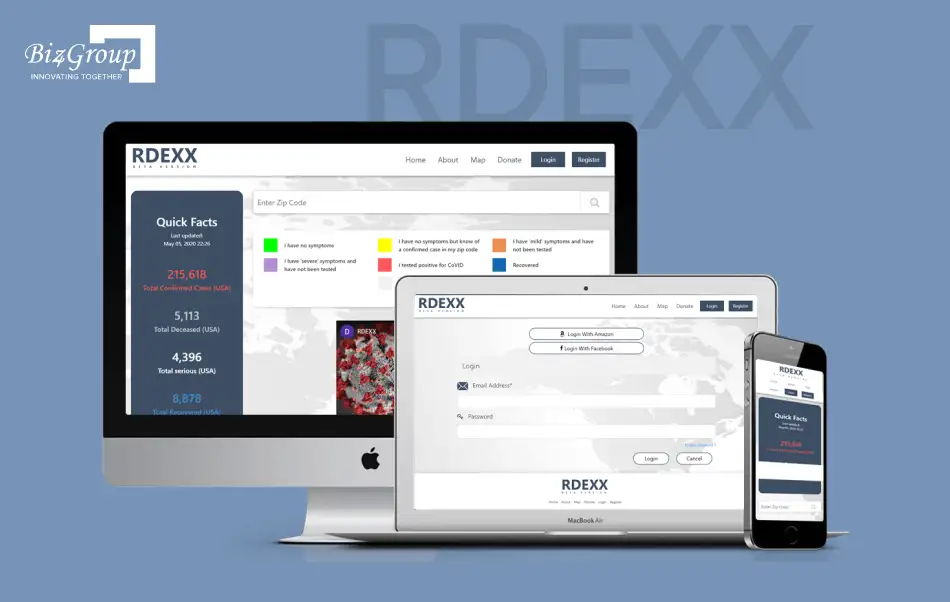
During the pandemic, we built RdeXX, a web-based platform for a leading healthcare brand that tracked and visualized global disease spread using live data analytics and geospatial mapping. The platform used AI to process thousands of health reports per minute, identify emerging clusters, and forecast high-risk zones, all in real time.
It empowered healthcare professionals and government agencies to plan responses faster, allocate resources intelligently, and curb disease transmission before it spiraled.
Now imagine combining that same predictive intelligence with billing systems, where real-time health trends inform coverage policies, claim volumes, and patient outcomes. This convergence of public health and billing data will reshape the very foundation of healthcare finance.
The future of AI medical billing software development is about smarter care. As AI becomes the backbone of revenue cycle management, systems like Biz4Group’s RdeXX and Dr. Truman’s AI Avatar show what’s possible when innovation meets intention.
At Biz4Group LLC, we build digital ecosystems that empower businesses to lead. We are a software development company in the USA, who intend to help entrepreneurs, startups, and enterprises create intelligent, future-ready solutions.
Our specialty lies in merging AI innovation with real-world functionality. From healthcare to manufacturing, fintech to fitness, we’ve delivered futuristic software that transforms ideas into scalable products. Our team of AI developers, UX strategists, data scientists, and compliance experts collaborates seamlessly to turn complex business problems into elegant, automated solutions.
When it comes to AI medical billing software development, we bring a rare blend of healthcare domain expertise and technical excellence. We understand that the healthcare industry is about trust, precision, and compliance. Every line of code we write reflects that responsibility.
Businesses across the USA (and beyond) partner with Biz4Group not because we promise success, but because we prove it. Here’s what makes us the development partner of choice for next-gen AI solutions:
Biz4Group is a team of thinkers, doers, and innovators who believe in building technology that actually changes how businesses operate. With our roots deep in innovation and our vision firmly set on the future, we’ve helped dozens of U.S.-based companies make intelligent medical billing software that not only automates claims but reshapes their financial performance.
In the evolving landscape of healthcare tech, having a partner that understands both AI and accountability can be the competitive edge that defines your success. Biz4Group delivers that edge with precision, speed, and credibility.
We know you’re ready to build an AI medical billing software that works smarter, earns faster, and scales confidently. Now, all you have to do is talk to Biz4Group.
Building an AI medical billing software is about reimagining the entire healthcare revenue cycle. From reducing human error and accelerating reimbursements to ensuring airtight compliance, AI empowers organizations to run smarter, leaner, and faster. As the healthcare industry continues to digitize, those who develop custom AI medical billing solutions for hospitals and clinics today will define the operational benchmarks of tomorrow.
The journey from idea to implementation may seem complex (data pipelines, compliance frameworks, and AI models can get overwhelming) but the outcome is worth every bit of effort. The right software can transform how billing teams operate, boost first-pass claim rates, cut costs, and drive consistent cash flow improvements. In a field where efficiency equals impact, the smart play is investing in automation that never sleeps and intelligence that keeps learning.
At Biz4Group, we’ve mastered the art of turning healthcare innovation into reality. With our proven expertise in AI medical billing software development, healthcare automation, and compliance-focused engineering, we’ve helped startups and enterprises across the USA bring their most ambitious ideas to life. Our finesse as an AI app development company leads us to code and craft intelligent, secure, and scalable systems that move the healthcare industry forward.
Let’s build your next big healthcare innovation together. The future of medical billing won’t wait, talk to Biz4Group today.
Development timelines depend on complexity, but typically, an MVP can be launched in 12–16 weeks, while a fully scaled AI-driven platform may take 6–9 months. Factors such as integrations, compliance, and custom AI training can extend timelines slightly.
Yes. Modern AI billing systems use APIs compatible with HL7 and FHIR standards, allowing smooth integration with most EHR and practice management systems without disrupting existing workflows.
AI models analyze historical claims and payer feedback to detect error patterns, missing codes, or documentation gaps before submission. This predictive approach can reduce denial rates by up to 60% and increase first-pass claim approvals significantly.
AI billing systems can be customized for any scale, from solo practitioners and small clinics to enterprise-level hospital networks. Cloud-based deployment makes it affordable and accessible for smaller healthcare providers.
Organizations typically see ROI within 6–12 months. Average results include a 25–40% reduction in operational costs, a 50% improvement in claim turnaround time, and measurable growth in revenue consistency.
AI models should be retrained every 3–6 months or whenever payer policies and coding standards change. Continuous learning ensures consistent accuracy and adaptability to evolving regulations.
with Biz4Group today!
Our website require some cookies to function properly. Read our privacy policy to know more.