Imagine a digital system that doesn’t wait for instructions but instead, understands your business goals, learns from real-time feedback, and takes independent actions to get the job done.
Read More

What if your electronic health record could do more than just store patient data?
What if it could actively predict risks, recommend personalized treatments, and streamline workflows in real time?
This is the promise of integrating AI with EHR/EMR systems, and it is already reshaping how healthcare organizations operate.
According to Markets and Markets, the global AI in healthcare market is projected to reach USD 21.66 billion in 2025 and grow to USD 110.61 billion by 2030 at a CAGR of 38.6%. At the same time, a Blue Prism survey revealed that 86% of healthcare organizations are already using AI in some capacity.
The challenge is that most of these AI applications remain isolated in imaging, billing, or administrative tools. The real transformation begins when AI is integrated directly into EHR/EMR systems, creating smarter decision-making capabilities, improving efficiency, and driving better patient outcomes across the care continuum.
For leaders considering adoption, exploring specialized AI healthcare solutions is often the first step toward understanding where AI delivers the highest value. From there, working with an AI development company experienced in EHR/EMR integration ensures that the implementation is both scalable and secure. And for organizations seeking long-term adaptability, choosing custom healthcare software development helps tailor these integrations to unique operational needs.
This blog will serve as a complete guide on how to integrate AI with EHR and EMR systems to transform healthcare operations. It will cover the “why” behind AI-EHR integration, the practical ways to make it work, real-world benefits, use cases, and everything related.
So let’s dive right into it!
For most healthcare executives, the real challenge is making sure that technology actually improves care delivery and streamlines operations. Traditional EHR/EMR systems have become essential record-keeping tools, but they rarely help leaders answer the bigger questions:
How can we reduce physician burnout? How do we catch patient risks before they escalate? And how do we keep the organization financially sustainable while improving patient satisfaction?
This is where AI integration steps in:
AI woven into EHR/EMR software can recognize trends across a patient’s history that may otherwise be overlooked. Imagine a physician receiving an alert that highlights early risk factors for readmission before discharge decisions are made. It is not just about data, it is about giving your care teams an extra layer of intelligence to act with more confidence.
One of the biggest frustrations for providers is the hours spent on paperwork. With AI assisting in medical coding and clinical documentation, physicians can focus more on their patients and less on typing. Partnering with a custom software development company ensures these integrations are tailored to your workflows, reducing friction and maximizing adoption.
Patients no longer want to wait for weeks to receive updates or struggle to schedule appointments. With AI-enabled chatbots connected to EHR systems, scheduling, reminders, and follow-up questions can happen instantly. Healthcare organizations exploring AI chatbot integration are finding it an effective way to make patient communication more natural and timely.
Healthcare is not just clinical, it is also about managing resources, staff, and budgets. AI-driven insights help identify where bottlenecks occur, whether it is underutilized staff hours or delayed claims. Leaders can make operational decisions with the same confidence they apply to clinical strategies, knowing they have evidence-backed insights at hand.
Integrating AI into EHR/EMR systems is not only about fixing today’s problems, it is about preparing for tomorrow. Organizations that move early gain experience, refine their systems, and set themselves apart as forward-thinking providers. Those who wait risk falling behind as patient expectations and industry standards continue to rise.
Bringing AI and EHR systems together is less about technology for its own sake and more about creating an ecosystem where clinicians, administrators, and patients all benefit. The next step is to look at the different approaches organizations can take to bring this integration to life.
Understanding the value of AI is one step, but figuring out how to bring it into an existing EHR or EMR system is where many leaders pause. The options can feel overwhelming, and the right approach depends on your priorities: speed, compliance, cost, or scalability. What matters most is choosing a path that strengthens your organization’s ability to deliver better care without overcomplicating daily operations.
|
Approach |
Description |
Best For |
|
API-Based Integration |
Connects AI tools directly to your EHR through secure APIs, adding features like predictive alerts or automation. |
Organizations looking for quick wins while keeping their current system intact. |
|
Native AI Modules |
Built-in AI features offered by some EHR vendors, such as automated coding or risk prediction. |
Providers already working with enterprise vendors like Epic or Cerner. |
|
Custom AI Solutions |
Solutions tailored around your workflows and patient needs, designed to solve specific challenges. |
Healthcare systems with unique requirements that standard tools cannot address. |
|
Cloud vs On-Premise |
Cloud deployment offers flexibility and scalability, while on-premise provides more direct control over sensitive data. |
Leaders balancing security and agility in their operations. |
|
Advanced AI Models |
Use cases that involve generative AI or specialized model development for tasks like conversational assistants or predictive charting. |
Organizations seeking to innovate and stand out in a competitive healthcare market. |
Some healthcare executives prefer to start small with API-based integrations, while others choose to invest in more tailored solutions that align with long-term strategy. In both cases, partnering with experts who provide AI integration services can reduce risks and accelerate results. For leaders looking further ahead, adopting enterprise AI solutions offers the opportunity to move beyond basic automation toward deeper transformation.
Once the method of integration is clear, the next step is understanding what these choices actually deliver in practice. That is where the benefits of AI-EHR/EMR integration begin to take shape.
Integrate AI with your EHR/EMR system to improve workflows, reduce errors, and support clinicians with real-time insights.
Start My AI Integration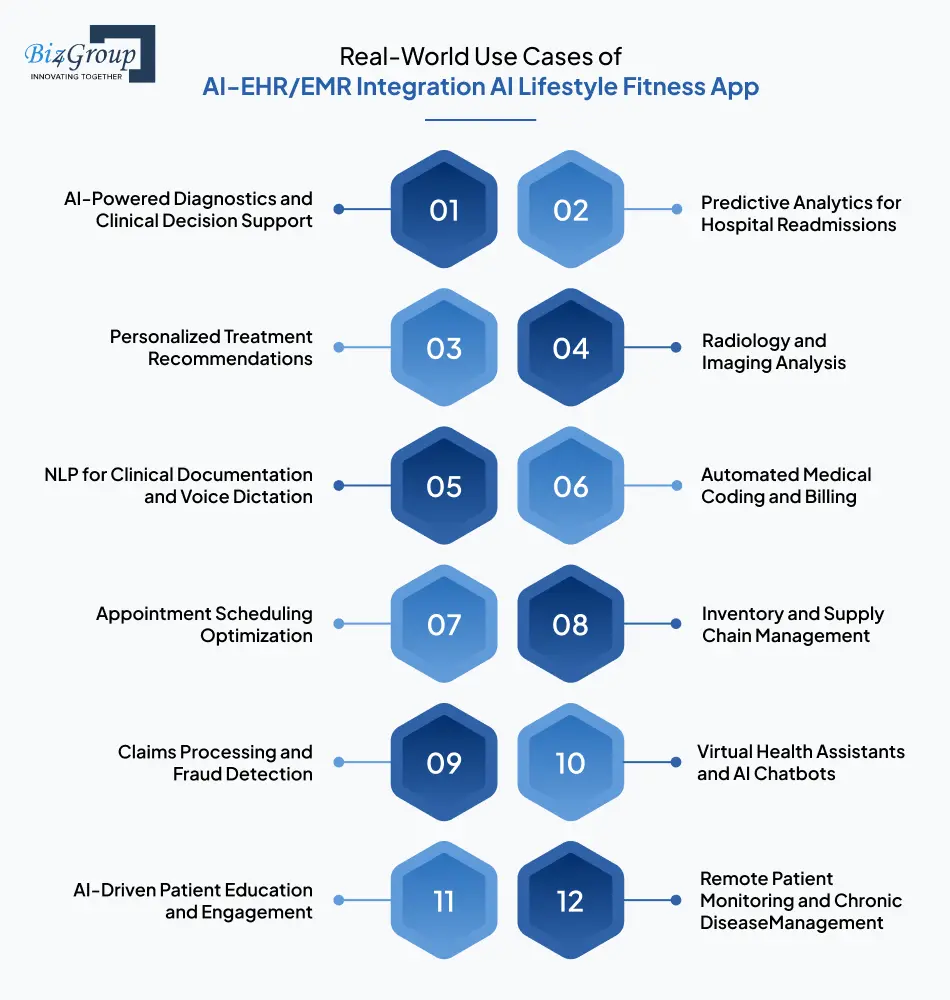
Integrating AI with EHR and EMR systems is no longer experimental. It is already shaping how leading healthcare providers manage operations, enhance care quality, and improve patient engagement. By embedding AI into everyday workflows, organizations are seeing measurable results that align with both clinical and business priorities. Below are some practical use cases, each backed by real-world adoption:
Clinical Use Cases
When patient data, imaging, and medical history are combined with AI inside EHR workflows, providers gain more timely and accurate insights. This reduces diagnostic delays, builds physician confidence, and helps improve patient safety.
AI integrated with EMRs can predict which patients are most likely to be readmitted after discharge. This enables proactive interventions, coordinated follow-ups, and reduced financial penalties from insurers.
AI-enabled EHRs create care plans that consider patient-specific data, from genetics to lifestyle patterns. This reduces reliance on one-size-fits-all treatments and supports precision medicine across specialties.
AI applied to imaging data within EMRs helps radiologists detect abnormalities more quickly and accurately. This reduces reporting delays and ensures patients receive faster access to life-saving care.
Natural language processing in EHR systems lets clinicians dictate notes that are automatically converted into structured records. This reduces administrative strain and gives providers more patient-facing time.
Administrative and Operational Use Cases
AI-driven coding systems integrated with EMRs reduce errors, speed up claim submission, and minimize reimbursement delays. This creates more predictable financial outcomes for healthcare organizations.
AI-powered scheduling within EHR systems helps balance physician availability with patient needs while predicting cancellations. This ensures fewer no-shows, better access, and higher operational efficiency.
AI connected to EMR workflows forecasts supply requirements based on procedure schedules and patient volumes. This prevents stockouts, reduces wastage, and helps cut procurement costs.
AI integrated into EMR-linked billing systems detects suspicious or irregular claim entries before submission. This strengthens compliance, reduces fraud risk, and accelerates payment timelines.
Patient Engagement and Experience Use Cases
AI-powered chatbots integrated with EHR systems handle appointment reminders, symptom check-ins, and basic patient questions. This reduces staff workloads while making care more accessible.
Conversational AI tools connected to EHRs deliver patient-specific educational materials. By making guidance personalized and actionable, adherence rates and overall outcomes improve significantly.
Wearables and remote devices feeding into AI-enabled EHRs give clinicians continuous patient insights. Early detection allows interventions before conditions worsen, lowering emergency admissions.
These examples demonstrate that AI-EHR/EMR integration is all about building a foundation for smarter care, stronger operations, and deeper patient engagement. Having said that, now let’s check out the step by step process of integrating AI in EHR/EMR.
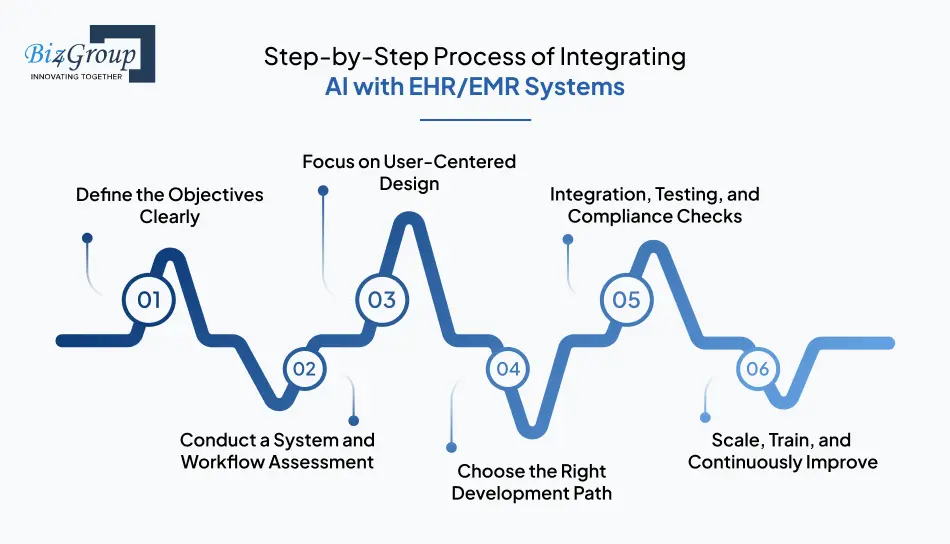
Integrating AI into EHR and EMR systems is a transformation that impacts workflows, compliance, and patient experience. Every stage should reduce risk inside your EHR environment, fit seamlessly into existing workflows, and support long-term adoption. If you are considering components that connect directly to your EHR, here is a guide on how to integrate seamlessly:
Healthcare leaders must pinpoint what they expect from AI-EHR integration—whether reducing administrative work, improving diagnostic speed, or increasing patient satisfaction. Without clear objectives, the project risks becoming fragmented and less impactful.
Each organization uses its EHR system differently, which means integration strategies vary. Evaluating current workflows, interoperability gaps, and compliance requirements ensures that AI is solving the right problems.
Even powerful AI tools can fail if clinicians find them hard to use. The interface must feel native within the EHR so staff don’t need to switch screens or retrain habits. Thoughtful collaboration with UI/UX experts ensures AI is intuitive, non-intrusive, and trusted by end-users.
Also read: Top UI/UX design companies in USA
Organizations must decide between vendor AI modules, API-based integrations, or fully customized solutions. Many leaders begin with an MVP embedded into their EHR to validate one use case before scaling further. MVP services enable testing in real-world workflows while limiting risk and cost.
Also read: Custom MVP software development
Integration must happen inside a safe EHR sandbox before moving into live environments. This ensures secure APIs, compliant data flows, and reliable performance without disrupting patient care.
Also Read: Software Testing Companies in USA
After proving success in pilots, AI solutions should be scaled across specialties while maintaining EHR consistency. Role-based training ensures adoption, while feedback loops refine performance continuously.
Leaders who treat AI-EHR/EMR integration as a structured process, not a one-off project, create systems that are reliable, compliant, and future-ready. With a process in place, the conversation naturally shifts to the compliance part that needs to be as robust as possible.
From predictive analytics to automated documentation, see how AI in EHR/EMR can transform clinical operations.
Explore My AI Healthcare SolutionIntegrating AI into EHR/EMR systems comes with extraordinary potential, but also heightened responsibility. Healthcare leaders must ensure that innovation never outpaces compliance. Regulatory frameworks, patient consent, and data privacy are not afterthoughts. They are the foundation that determines whether AI integration is sustainable and trusted.
In the U.S., HIPAA compliance remains non-negotiable, but organizations must also consider GDPR in Europe and other regional laws. AI-EHR integration requires strict handling of protected health information (PHI) with clear audit trails. Non-compliance risks fines and can erode public trust at scale.
Patients want to know how their health data is being used, and AI brings new layers of complexity. Building transparency into the consent process ensures patients feel safe when their data powers predictive models or diagnostic tools. Consent forms should explicitly cover AI-driven workflows.
EHR systems integrated with AI must use encryption, access controls, and secure APIs to prevent breaches. Beyond compliance, strong safeguards create confidence for stakeholders who approve funding and for patients whose data drives the system. Leaders often choose to hire AI developers with healthcare expertise to strengthen these safeguards.
AI models used in EHR systems must be explainable and auditable. If a model recommends a treatment path or flags a risk, organizations must be able to justify those decisions under scrutiny from both regulators and patients. A black-box approach creates legal and ethical vulnerabilities.
When working with external vendors or API providers, their compliance posture becomes your responsibility. Leaders should carefully vet contracts, ensuring vendors meet HIPAA, GDPR, and FDA guidelines for AI-enabled medical tools. Trustworthy vendors reduce the risk of compliance gaps.
Regulatory environments evolve quickly, and what is acceptable today may be outdated tomorrow. Healthcare organizations must commit to ongoing audits and policy reviews. Tools that integrate AI into an app or existing systems often require updates to stay aligned with new regulations and market best practices.
With compliance as the backbone, leaders can then turn their attention to another crucial dimension: the ethical considerations of AI in healthcare.
When AI is embedded into EHR and EMR systems, the conversation extends beyond compliance into ethics. Leaders must ask not only “is this allowed?” but also “is this the right thing to do for patients, clinicians, and society?” Ethical considerations shape whether AI earns trust, drives adoption, and creates long-term value in healthcare.
AI trained on limited or skewed data can unintentionally reinforce disparities in healthcare. Leaders must insist on diverse datasets and continuous audits to ensure AI-driven recommendations are fair to every patient group. Equity cannot be an afterthought if healthcare is to remain patient-centered.
AI should never replace the empathy and intuition of physicians. Instead, it should free them from administrative burdens so they can focus on human connection. Designing systems that enhance rather than diminish personal care is vital for patient trust.
When AI models influence treatment paths or flag patient risks, clinicians must understand the reasoning behind those outputs. Black-box recommendations can erode confidence, while explainable systems support trust and accountability across the care continuum.
Generative AI opens opportunities for patient education, predictive charting, and conversational support inside EHRs. However, without guardrails, it can introduce misinformation or produce errors. Partnering with experts in generative AI helps ensure responsible design and safe deployment in sensitive environments.
Patients should feel ownership of their data and have the ability to consent to AI-driven applications. Providing clear explanations about how AI interacts with their EHR empowers them to remain active participants in their own care.
While AI enhances efficiency, leaders must guard against staff deferring entirely to automated outputs. Embedding checks that require clinician oversight ensures AI remains a tool rather than a decision-maker. This balance protects both medical judgment and patient safety.
EHR-linked AI should deliver insights in ways that empower patients rather than overwhelm them. Thoughtful design of conversational platforms, such as an AI conversation app, ensures patients receive information that is accurate, understandable, and respectful.
Healthcare organizations that prioritize fairness, transparency, and human-centered design will lead the industry in both trust and outcomes. With these ethical principles in mind, leaders can now look at another dimension of AI integration: the financial investment and cost considerations that determine its scalability.
The cost of integrating AI into EHR/EMR systems generally falls between $20,000 and $150,000+, depending on scope, complexity, and compliance requirements. Smaller pilot projects usually sit at the lower end, while large-scale deployments with multiple AI features and stricter compliance needs reach the higher range.
|
AI Integration Component |
Estimated Range (USD) |
Details for Healthcare Leaders |
|
AI Model Development for Healthcare Data |
$15,000 – $40,000 |
Building models that handle clinical notes, predictive analytics for patient risks, or generative AI for summaries and recommendations. |
|
EHR/EMR System Integration of AI Modules |
$20,000 – $50,000 |
Creating APIs, middleware, and workflows so AI features (like chatbots or decision support) work seamlessly within existing EHR/EMR systems. |
|
Data Preparation and Normalization for AI |
$5,000 – $15,000 |
Cleaning, structuring, and de-biasing patient data to ensure AI delivers accurate, ethical, and reliable insights. |
|
Regulatory Compliance for AI-Driven EHR/EMR |
$10,000 – $25,000 |
Implementing HIPAA, GDPR, and FDA safeguards such as encryption, audit logs, and role-based access to protect AI-powered workflows. |
|
AI Feature Interface Design for Clinicians |
$5,000 – $15,000 |
Designing intuitive dashboards and alerts so doctors and staff can easily use AI outputs inside their daily EHR/EMR workflows. |
|
Pilot Deployment of AI Features in EHR/EMR |
$10,000 – $30,000 |
Limited rollout of AI-powered features (like automated coding or clinical decision support) to validate before scaling across the organization. |
|
Ongoing AI Model Monitoring and Updates |
$5,000 – $20,000 annually |
Retraining AI models, updating algorithms, and adapting to evolving compliance requirements to ensure sustained performance. |
Even at the higher end, healthcare organizations often find the ROI significant, as AI-driven EHR systems reduce administrative load, improve patient safety, and optimize resource use. Once leaders understand the cost landscape, the next step is preparing for the challenges that can emerge during integration and how to solve them.
Also Read: Cost of Implementing AI in Healthcare
Adopt AI-EHR integration that meets HIPAA, GDPR, and FDA standards while boosting patient trust and safety.
Build My AI-Ready EHR Syste mWhile the promise of AI in EHR/EMR systems is transformative, leaders often face obstacles that can delay or derail progress. These challenges happen to touch people, budgets, workflows, and trust. Understanding them upfront and knowing how to navigate them allows healthcare organizations to move from hesitation to confident adoption.
|
Common Challenges |
How to Solve |
|
Integrating AI into EHR systems can demand significant investment in custom development, upgrades, and specialized expertise. |
Begin with phased rollouts and an MVP to validate ROI before scaling. Partnering with experts in business app development using AI helps control costs. |
|
Healthcare data often exists in silos across departments and third-party systems, making it difficult to centralize and apply AI effectively. |
Adopt interoperability standards like HL7 FHIR and build structured data pipelines. AI-enabled middleware can ensure that EHRs pull from a single, trusted data source. |
|
Clinicians may worry that AI tools will complicate workflows or undermine their professional judgment. |
Involve care teams early in the design process, focus AI features on reducing workload, and provide pilot programs with training to build trust. |
|
Patient data can be exposed to risks if integration is rushed or security protocols are inconsistent. |
Implement HIPAA-compliant encryption, role-based access, and continuous monitoring via a trusted software development company in Florida. |
|
Evolving regulations leave leaders uncertain about how AI should be used responsibly in healthcare. |
Conduct regular compliance reviews and design systems with flexibility so updates can be made as laws change. |
|
AI tools may work well in one specialty but fail to scale smoothly across departments or sites. |
Use a modular approach that allows incremental deployments, ensuring each rollout is tested and refined before expansion. |
|
Poorly trained AI models can reinforce bias or produce inaccurate recommendations. |
Monitor AI outputs regularly, retrain with diverse datasets, and embed oversight mechanisms to support clinician review. |
Every challenge is also an opportunity for leaders to strengthen their systems, build trust with clinicians, and improve patient outcomes. Once these hurdles are addressed, the conversation naturally shifts to another critical question: how to identify and mitigate bias in AI models and patient data.
When AI becomes part of EHR and EMR systems, leaders need to ensure that predictions and recommendations serve every patient group equally. Addressing this challenge upfront builds trust and makes integration more sustainable.
AI trained on limited patient records often struggles to reflect the diversity of real-world populations. Expanding datasets across age groups, ethnicities, and geographies reduces blind spots and helps ensure that outputs reflect the patients your organization actually serves. The top AI development companies in Florida, can guide this process with proven methods for curating balanced data.
Bias does not stay static. As new data flows into EHR systems, AI models can drift in their predictions. Regular reviews and recalibrations help organizations detect bias early and prevent it from shaping care decisions over time.
No algorithm can fully replace human context. Creating oversight loops where clinicians review AI outputs ensures that questionable recommendations are challenged before they reach patients. This collaboration strengthens trust in both the technology and the outcomes it supports.
If clinicians cannot understand how a model reached its conclusion, they cannot reliably spot bias. Choosing explainable AI tools within EHR systems helps decision-makers trace reasoning and catch irregularities before they affect patient care.
Sometimes bias stems from socioeconomic or cultural gaps, not just medical records. For instance, predictive models may unintentionally favor groups with better historical access to healthcare. Leaders should evaluate these broader impacts and adjust algorithms to avoid reinforcing inequities.
The way information appears inside an EHR matters. Alerts that emphasize certain patient groups over others may unintentionally skew decisions. Applying thoughtful design practices, such as those seen in AI assistant app design, helps ensure outputs are framed in a way that promotes fairness.
Bias may never be eliminated completely, but it can be managed responsibly with the right mix of data, oversight, and design. By making fairness a guiding principle, healthcare leaders can integrate AI into EHR systems with confidence.
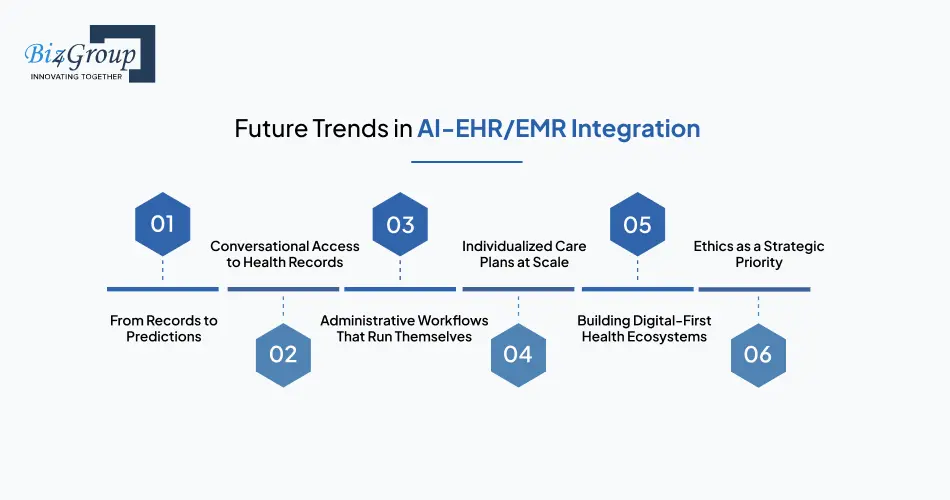
The integration of AI with EHR and EMR systems is still in motion, but the real value for healthcare leaders lies in anticipating what comes next. The future will not simply be about faster systems but about rethinking how healthcare is delivered, managed, and experienced.
EHRs will no longer just capture what has happened. AI will push them toward forecasting health events before they occur. Imagine systems that can flag a patient’s risk of readmission weeks in advance, enabling care teams to intervene early and prevent costly complications.
AI will give patients and clinicians new ways to interact with data. Instead of navigating complex dashboards, future EHRs may respond to natural language questions, offering insights through conversational interfaces. The groundwork is already being laid with chatbot development for healthcare industry, which will only grow in sophistication.
In the near future, many back-office tasks may require little to no human input. Scheduling, billing, and documentation could be fully automated by AI embedded within EHRs, freeing up staff time and reducing operational bottlenecks. Leaders who plan for this shift today will see significant efficiency gains tomorrow.
As datasets expand and AI becomes more refined, EHR systems will be able to move from generalized treatment suggestions to deeply personalized pathways. Future integrations may consider everything from a patient’s genetics to their environment, reshaping how care plans are built and delivered.
EHRs will not just sit at the center of a hospital—they will connect the entire care journey. We can expect AI-enabled systems to link virtual consultations, diagnostics, and follow-ups into one connected digital environment, supported by innovations in AI medical web development.
Future success will not be measured by technology alone but by how responsibly it is applied. Organizations that prioritize fairness, patient consent, and transparency in their AI-EHR integrations will stand out, both in reputation and in long-term adoption.
For healthcare executives, these trends are less about chasing technology and more about preparing for a landscape where AI quietly transforms daily operations. With the future unfolding this way, it becomes equally important to ask: which partner is best positioned to help bring this vision to life?
Selecting the right partner for AI integration with EHR/EMR systems is a decision that impacts every layer of your healthcare organization - from clinician satisfaction to patient outcomes. Biz4Group has worked with forward-thinking healthcare providers to design, build, and scale solutions that not only meet today’s needs but prepare for tomorrow’s challenges.
Our work includes building several innovative AI platforms like Semuto, which delivers personalized wellness recommendations.
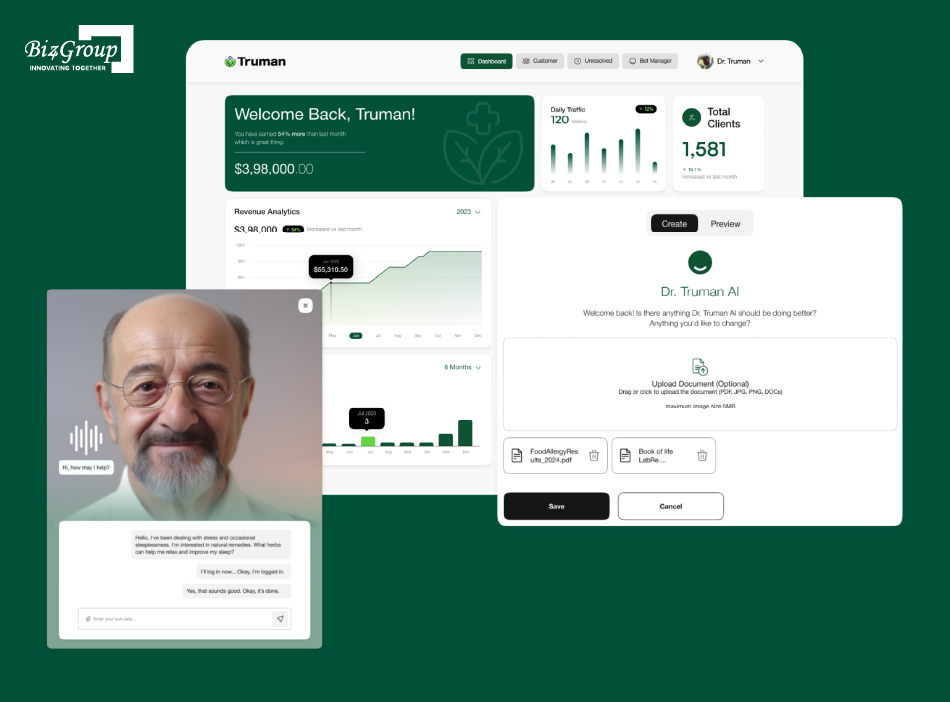
Truman, on the other hand, is an AI-enabled health companion with a virtual avatar for immersive patient engagement.
Projects like these show our ability to blend AI with healthcare data in ways that improve usability and trust. This same expertise translates seamlessly when integrating AI into EHR/EMR systems, where personalization and patient experience are just as critical.
Instead of offering one-size-fits-all tools, we build custom modules that connect seamlessly with your existing EHR environment. As an AI app development company, our focus is on solutions that are practical, scalable, and aligned with your goals.
From HIPAA to GDPR, our integration strategies are built with regulatory standards in mind. You can trust that privacy, security, and transparency are part of the design—not add-ons.
We focus on making AI tools usable for clinicians and administrators. By prioritizing intuitive design, our solutions reduce resistance and drive adoption across departments.
From strategy to development and post-launch support, Biz4Group stands beside healthcare leaders throughout the journey. This ensures smooth rollouts and long-term success without disruptions.
Choosing Biz4Group means working with a partner who sees AI-EHR integration not as a technical challenge but as a strategic opportunity for your organization. With the right approach, your systems can evolve into powerful tools that improve efficiency, enhance patient care, and prepare you for the future of healthcare.
Turn integration challenges into opportunities with tailored AI models that work for your healthcare organization.
Solve My AI Integration ChallengesThe future of healthcare will not be shaped by paper charts or clunky dashboards. It will come from how seamlessly AI works inside the EHR and EMR systems that clinicians and patients use every day. Whether it is reducing routine paperwork or helping predict risks before they surface, AI-EHR integration is steadily moving from being an option to becoming a necessity.
For decision-makers, the focus now is not whether AI fits into healthcare systems but how to make it work in ways that are ethical, efficient, and impactful. If you are exploring how to build AI software that can improve patient care and operational flow, choosing the right AI product development company becomes the key step in turning ideas into solutions that last.
See what tailored AI integration could look like for your organization.
The timeline depends on the complexity of the healthcare organization, the number of systems involved, and the type of AI solution being implemented. While smaller pilots may take a few months, large-scale integrations often span over a year.
Predictive analytics models, natural language processing (NLP), and machine learning classifiers are commonly applied. Each serves a different purpose, from forecasting patient risks to converting unstructured notes into actionable insights.
Yes, but it requires careful planning. Many healthcare organizations layer AI through APIs or middleware to bridge gaps with older systems rather than replacing them outright.
Initially, there may be a learning curve. However, once adoption grows, AI reduces repetitive tasks like documentation and scheduling, freeing clinicians to spend more time on direct patient care.
The main risks are privacy breaches and model inaccuracies. Both can be mitigated through strong compliance frameworks, continuous monitoring, and clear oversight mechanisms.
It is unlikely that AI will replace core EHR functions. Instead, it will enhance them by making processes faster, smarter, and more personalized without removing the foundational record-keeping elements.
with Biz4Group today!
Our website require some cookies to function properly. Read our privacy policy to know more.